
The Mechanism of Action of Mebendazole
Mebendazole is an important potent anthelmintic drug in the treatment of parasitic worm infestations, both single and mixed. This essay shall elaborate on the mechanism of action of Mebendazole and try to explain how this active chemical effectively combats these unwelcome intruders in humans. It acts specifically on the cytoplasmic microtubules of the intestinal cells of worms, leading to their demise. It is a known fact that the absorption of Mebendazole increases with fatty food, making it an important consideration for efficacy optimization.
The paper will also provide an overview of this drug, including administration and dosing. Extended discussions will focus on the clinical studies that supported its use and the adverse reactions to watch out for, such as elevated liver enzymes and serious skin reactions. Major considerations for its drug interaction, contraindications, and special population considerations, particularly during pregnancy and lactation, will also be explored. Hence, the article aims to provide deep insights into the pivotal role Mebendazole plays as a cornerstone in the pharmaceutical arsenal against parasites, underlining its significance in the current global health scenario.

Mebendazole Description
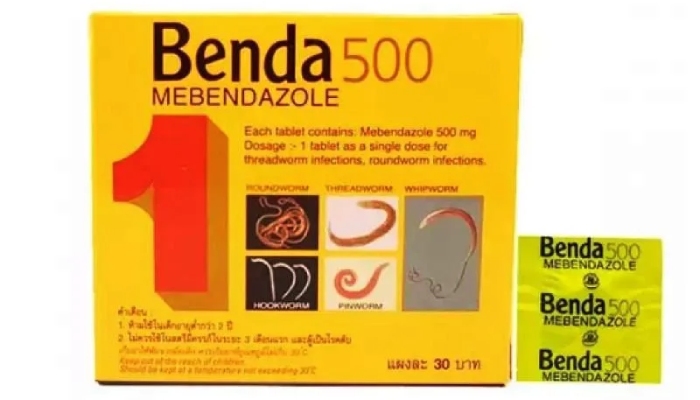
Mebendazole is a cornerstone in the therapy of parasitic infections, effective against both single and mixed infections due to its broad anthelmintic properties. It targets a wide range of parasitic worms that belong to the benzimidazole class, including those causing hookworm, roundworm, whipworm, and pinworm infections. Mebendazole’s mode of action involves the inhibition of tubulin polymerization into cytoplasmic microtubules, which are crucial for glucose uptake and cellular processes like division and growth, ultimately leading to parasite death.
The drug is available in oral dosage forms, such as tablets and chewable tablets, suitable for both adults and children. The bioavailability of Mebendazole can be increased when administered with fatty foods, enhancing absorption efficiency. Mebendazole is administered at doses measured in mg/kg, reaching effective plasma concentrations necessary to impact the parasite’s survival. However, caution is required in patients with impaired hepatic function, as elevated liver enzymes and liver function tests may indicate hepatic impairment. The unchanged drug, considering its effects on the liver, underscores the need for careful monitoring, especially in treatments involving higher doses than a single-dose regimen. This strategic application of Mebendazole significantly aids in the management of parasitic infections, underscoring its vital role in modern pharmacology.
Mode of Action
The key to fighting single and mixed parasitic diseases lies in the innovative mode of action of Mebendazole. This medication selectively inhibits the synthesis of microtubules, essential for the development and survival of parasitic worms, thereby disrupting their absorption of vital nutrients. This mechanism effectively starves the parasites, leading to their paralysis and eventual demise. Mebendazole is administered as a single oral dose, tailored in mg/kg to maximize efficacy while minimizing side effects. Its oral dosage form, encompassing tablets and chewable tablets, ensures targeted delivery to the gastrointestinal tract, precisely where it’s needed, without adversely affecting the host’s cells.
A notable aspect of Mebendazole’s clinical pharmacology is that fatty food increases absorption of the medication, likely enhancing its therapeutic effect. However, it’s important for patients to be vigilant about the rare possibility of serious skin reactions, necessitating immediate medical intervention. The drug’s excretion into human milk remains underdocumented, urging caution during treatment of nursing mothers. Given its broad mechanism of action and the benefit of increased absorption with fatty food, Mebendazole stands out as an exceptionally effective anthelmintic agent against a diverse array of parasitic infestations.”
Mebendazole Dosage and Administration
In respect to this, it is very important that individual dosages and administration of Mebendazole be done in such a manner that the drug is administered at the least effective dose but with the least side effects associated. In the treatment of single or mixed infections, the standard regime is 100 mg, two times daily, for three successive days. This is applicable to adult people and children above 2 years of age, with adjustments made considering the type and severity of the infection, and patient-related factors such as age and body weight. Conditions being treated may require prolonged therapy with Mebendazole, sometimes at high dosages, before a clinical cure is effected.
Mebendazole is given orally, either as tablets or chewable forms, with or without meals. However, when taken with fatty foods, there may be an increase in absorption and thus likely enhancement of the medicine’s effectiveness. Patients are strongly recommended to adhere to the given dosage and course of treatment in order to get the best results. The course can be repeated in cases where the infestation is high to ensure the total eradication of the infection. The drug may be taken with a small amount of food, which tends to improve its absorption into the bloodstream, more so in the chewable tablet, since this is easily administered even to young children or those having difficulty swallowing tablets. Ensuring normal hepatic function is also essential, as Mebendazole’s metabolism is hepatic-dependent.

Clinical Studies With Mebendazole Chewable 500 mg Tablet
Clinical trials have largely helped establish the effectiveness and safety profiles of the Mebendazole Chewable 500 mg Tablet in various parasitic infestations, proving to kill parasites of several types. In key clinical trials, it has been demonstrated that patients treated with Mebendazole Chewable 500 mg tablet have improved symptoms of soil-transmitted helminths, including those associated with Ascaris, Trichuris, and hookworm infections, resulting in a significant reduction in worm burden. Further studies in this area resulted in finding the impact of treatment on school-aged children in regions that bear a high prevalence of intestinal parasites.
They concluded that it was beneficial not only in bringing down the prevalence of gastrointestinal infections but also in improving the nutritional status and cognitive development of the children; this was associated with the use of single oral doses of Mebendazole Chewable 500 mg Tablet. Effective immobility and death of the parasites resulted from the complete inhibition of the cytoplasmic microtubules, one of the essential actions implicated in the successful efficacy of the drug. It was also noted that when taken with fatty food, it might even contribute to increasing the drug’s absorption, hence possibly resulting in enhanced drug efficacy. In particular, the safety profile of the tablet was evaluated very closely. The results showed that any adverse effects were minor and transient, thereby further confirming the suitability of the drug to be indicated in the treatment of parasitic infections.
MEBENDAZOLE TABLETS, USP
MEBENDAZOLE TABLETS, USP, represent a vital oral pharmaceutical preparation in the arsenal against parasitic worm infections, meeting rigorous USP dissolution criteria for quality, purity, and strength. These tablets are carefully designed to ensure that patients receive a consistent, uniform, and effective dose for treating a range of parasitic conditions. The active ingredient in Mebendazole disrupts microtubulin formation within parasitic worms, effectively leading to their demise.
With USP certification, these tablets guarantee quality and safety after undergoing stringent tests and verification processes. Available in 100mg and 500mg dosages, Mebendazole offers flexible dosing options for infections such as hookworm, roundworm, whipworm, and pinworm. It is important to note that the absorption of Mebendazole can be significantly increased when the medication is taken with fatty food, thus potentially enhancing its effectiveness against parasitic infections. Therefore, Mebendazole Tablets, USP, are a cornerstone in the therapeutic armamentarium against parasitic infections, providing healthcare personnel and patients with a reliable and standardized treatment option.
3.4 Inhibition of mitochondrial reactions
Inhibition of Mitochondrial Reactions delves on the fact that Mebendazole has profound effects on the metabolic pathways of parasitic worms through a specific impact on the mitochondrial processes. The activity of mebendazole is attributed to the ability to perturb normal operation in the mitochondria, which is vital to the cells in the production of energy. Mebendazole acts by inhibiting some key enzymes in the mitochondrial electron transport chain that are involved in the capacity of the parasites to produce ATP, the cell’s energy currency. The action extends not only to the worm’s metabolism but also to the viability, growth, and reproduction of the worms. The repression of mitochondrial reactions is paramount in the mode of action with Mebendazole; it reduces the energy within the parasites to a point of immobilization and eventual death.
This mechanism gives the evidence for the selectivity of the drug, as the parasitic worms were killed at the expense of the host’s cells, which spares him because of differences in his mitochondrial biology compared to that of a parasite. Such findings reveal the action of Mebendazole in the functions of the mitochondria, explaining its broad-spectrum antiparasitic activity and emphasizing the importance of the mitochondrial ways as one of the therapeutic targets in the treatment.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity, mutagenicity, and impairment of fertility: studies on the possible effects of mebendazole required to be conducted in a very critical part of the safety appraisal. Mebendazole has been evaluated for its genotoxic potential in germ cells for mutagenic and/or clastogenic activity that could result in heritable genetic damage. Carcinogenicity: Some research concluded that, based on the duration of administration, the drug used at therapeutic dosages does not present a considerable risk with respect to its potential for causing carcinogenesis. Mutagenicity studies have also indicated that Mebendazole does not cause serious genetic mutations that might lead to cancer or any other genetic diseases.
All animal studies that tested doses of Mebendazole used for the treatment of parasitic infections showed no evidence of fertility impairment; therefore, the probability that human exposure might lead to any impairment of fertility is low. However, it should be kept in mind that all drugs have an innate specific level of risk, and hence the safety of oral dose of Mebendazole is under constant monitoring, even in the post-marketing period, for timely detection of any potential hazard and proper management in accordance.
Contraindications for Vermox
Contraindications are to be followed by Mebendazole (Vermox) with specifications in order not to compromise the patient’s security. The counter is not to be taken by persons known to be hypersensitive or allergic to mebendazole or any of the ingredients found in Vermox. Besides, Vermox is to be administered with cautiousness to patients with liver diseases, as it exaggerates derangement of liver function. Pregnant women are also cautioned while administering the tablets of Vermox, mostly during the first trimester of pregnancy since there is not enough study which has indicated it as safe to be used in pregnancy.
On the other side, Mebendazole is, however, considered to be safe for use in some populations, which include children and adults for the treatment of parasitic infections but are to be avoided from use where potential harms may outweigh its benefits. The health provider should screen through the patient’s medical history and current health status, with regards to the possible contraindications, before giving his opinion on the administration of mebendazole metabolism Vermox.
Uses for Vermox
Vermox (Mebendazole) is a very effective medicinal drug that is prescribed to a number of patients for the treatment of some kinds of helminthic infections. The most prevalent treatment is applied in curing soil-transmitted helminthiasis, where the medicine helps treat infections caused by hookworms, roundworms, whipworms, and pinworms. Vermox acts by the process of selective inhibition of the synthesis of microtubules in the parasitic worms, leading to the death of the worm.
This medicine is also applied for therapy in case of more complicated infections, such as trichinellosis, caused by people eating undercooked meat infected with the larvae of Trichinella spiralis. Besides what has been mentioned, Vermox also finds its use in the treatment of hydatid disease in some cases. It is used to treat gastrointestinal infections and those caused by the larva of the Echinococcus granulosus tapeworm, though applied very carefully in increased dosages. Vermox is, therefore, broadly appreciated due to its wide-range anthelmintic action and has a cardinal role in therapy throughout the world for helminth infections.

Risk Of Convulsions
Mebendazole should be given to a patient with a history of seizures and predisposition to the possible development of convulsions. Although Mebendazole is definitely safe in treatment against parasitic infections, some convulsions of epileptic predisposed persons with existing pathologies, or in cases of high doses, have been reported. The actual mechanism leading to such convulsions is not well understood, but it might be in relation to the action of the drug on the parasite’s nervous system, and, secondarily, on the nervous activity of the host.
It should be administered with caution to patients known to have seizure disorders, with due warning to healthcare providers and proper observation of neurological adverse effects. In high-risk patients for convulsions, other than these drugs should be considered in order to minimize the possibility of adverse outcomes.
1.3 Effects During Pregnancy and Lactation
Pregnancy
Use of Mebendazole in pregnancy should be taken with great caution, especially in the first trimester, because it has no definitive studies concerning the safety of the developing fetus. Animal studies have not demonstrated any damage, but human data is not sufficient. Healthcare providers should assess the potential benefits for the pregnant woman against the likely risks for the fetus before initiating therapy to parasitic infections. If Mebendazole therapy is not avoidable, it should be conducted under strict medical supervision.
Lactation
Excreted in breast milk but not excreted in sufficient amounts; there is no enough data that documents the excretion of the drug in breast milk with regard to lactation, where the excretion may take place. There is scant caution is needed when considering the administration of mebendazole to a nursing mother. Whether breastfeeding is to be stopped or continued during therapy with oral mebendazole, should be at the discretion of the healthcare provider after weighing the risks to the baby against the benefits the baby may derive from being breastfed. In these situations, treatment may be withheld until the patient completes her duration of breastfeeding, or the prescriber may decide upon safer alternatives for use during lactation.
Drug Interactions for Vermox
Concomitant Medications
It is of moderate risk to have drug interaction of Vermox (Mebendazole) with other drugs. In particular, Vermox may interact with those drugs which would induce liver enzymes, for the reason that the liver enzymes are required to metabolize Mebendazole. For example, inhibitors of these enzymes might increase the level of Mebendazole in the blood, thereby possibly increasing efficacy or toxic effects. On the other hand, inducers of these enzymes may lower the effectiveness of Mebendazole.
Impact on Other Treatments
Vermox can also modify the pharmacokinetics of other drugs: their absorption, distribution, metabolism, or excretion. For example, some antiepileptics or diabetes-controlling medications have interactions with Vermox and require some dose adjustments to them for maintaining their medicinal effectiveness levels appropriately. Health care providers are reminded to review all the medications patients may be taking to be able to make an assessment for any potential drug interactions and adjust treatment plans if indicated.
Monitoring and Management
Patients should be proactively checked for possible drug interactions, and in such cases, medication management should be done with Vermox. Health care providers need to thoroughly check all the medications being prescribed to their patients, including their consideration to reduce doses or substitute medications. Awareness should also be passed on to the patients in regard to these symptoms, along with timely patient-provider communication in case of such reactions or untoward effects following administration with Vermox.

Overdose Information for Vermox
The overdose information for Vermox tells of adherence to the dosages that one has been given to avoid the possible adverse effects associated with overdosing. In the event of a Vermox (Mebendazole) overdose, symptoms such as abdominal pain, diarrhea, vomiting, or other possible rare neurological signs like dizziness and convulsions can be expected. Treatment in case of Vermox overdose includes supportive measures like gastric lavage or activated charcoal to prevent further absorption of the drug.
Additionally, the patient should be closely monitored for any signs of toxicity, and symptomatic treatment should be provided if necessary. There is no specific antidote for Mebendazole overdose, thus symptomatic management and limiting further absorption of the drug remain central in the treatment strategy. Patients or their caretakers should be instructed on the importance of taking the medication exactly as prescribed and on the urgency of seeking medical attention promptly if an overdose is suspected.
Clinical Implications and Recommendations
Clinical Implications and Recommendations” emphasizes the main pragmatic implications of Mebendazole mechanisms. It implicates its effect on parasitic worms, translating into effective protocols in the treatment of hosts full of infections, among them, hookworm and roundworm. Recommendations for health providers highlight the importance of considering the effectiveness and safety of Mebendazole, especially since its application for use by sensitive groups such as pregnant women and children is guided by the latest clinical guidelines.
Furthermore, studies on parasitic worms have documented certain cases of resistance, underscoring the need for continued monitoring and suggesting alternative drugs or drug combinations to ensure activity is maintained. Future efforts should involve studies on the molecular basis of resistance mechanisms to develop better Mebendazole formulations or improved combination therapies. Additionally, education programs for health providers and patients will be established to optimize adherence to treatment protocols, thereby reducing the risk of resistance development and optimizing treatment success.
Ultimately, though Mebendazole remains one of the cornerstones of anthelmintic therapy in the treatment of parasitic infections, holistic management that incorporates patient education, guideline adherence, and constant research is crucial to optimizing its clinical benefits and minimizing challenges.
Conclusion
Finally, the importance of the drug Mebendazole in the treatment of parasitic infections is very crucial to the aspect of health worldwide. This unique mechanism of action provides an effective means by which not only a variety of parasitic worms can be fought but also ensures their effective eradication. Continuing research into the effects of Mebendazole, including potential resistance, administration during pregnancy, and lactation, calls for balanced administration. Health care professional and practitioners should keep abreast of the newest guidelines and research to ensure the best practice in treatments for their patients. With clinical implications and recommendations ensuring effective and safe use across diverse patient populations, Mebendazole is poised to maintain its role as a cornerstone in the fight against parasitic infections.
